ItŌĆÖs the dream of any young medical technology researcher: the chance to shepherd their work through the entire development process, starting in the research lab and ending with a product that makes a difference in the lives of patients around the world.
You might expect that for a student like Lee MacDonald, PhD candidate in program, such a dream would be years off ŌĆö at the very least sometime after completing his dissertation. In this case, though, youŌĆÖd be wrong: MacDonaldŌĆÖs research is poised to be implemented in cancer treatment across the globe within the next year.
On Wednesday, ┬ķČ╣┤½├Į announced the licensing of intellectual property developed by MacDonald, his supervisor Dr. Christopher Thomas and Dr. James Robar, director of DalŌĆÖs Medical Physics programs, to . The company, headquartered in Germany, is an international leader in software-driven medical technology, particularly in radiation oncology. Its advanced systems, which aim to offer less-invasive treatments, can be found more than 100 countries and in 75 per cent of the top 1,000 cancer treatment centres globally.

L-to-R: Sean Clark (president, Brainlab), Dr. Cristopher Thomas (assistant professor, Medical Physics), Lee MacDonald (PhD student, Medical Physics), Martha Crago (vice-president research), Dr. James Robar (director, Medical Physics programs).
Now, an algorithm developed by MacDonald and his collaborators will enable BrainlabŌĆÖs systems to deliver more precisely targeted radiation treatments to cancer patients, resulting in less damage to surrounding healthy organs and tissue.
ŌĆ£ItŌĆÖs so exciting just to see the application of all this work gather into something that can see real potential for patient benefit,ŌĆØ says MacDonald. ŌĆ£ThatŌĆÖs the goal of this work for us: seeing it implemented.ŌĆØ

Improved patient treatment
DalŌĆÖs Medical Physics offerings ŌĆö accredited last year by the Commission on Accreditation of Medical Physics Educational Programs (CAMPEP) ŌĆö include a masterŌĆÖs, a PhD and a certificate program. MacDonald is a graduate of the masterŌĆÖs program and is now in the second year of his PhD. HeŌĆÖs studying in a field that combines physics and medical research with a focus on patient care and treatment.
Read more:
ŌĆ£We feel very privileged, because we get to observe treatment delivery every day and identify shortcomings and opportunities, then feed those opportunities right back into our research,ŌĆØ says Dr. Robar, director of DalŌĆÖs Medical Physics programs and chief of the Department of Medical Physics with the Nova Scotia Health Authority. ŌĆ£This technology was really born out of that kind of experience.ŌĆØ
Approximately 53 per cent of cancer patients receive radiation treatment during the treatment and management of their disease. At facilities like the Nova Scotia Cancer Centre in Halifax, large linear accelerators, guided by state-of-the-art software, deliver advanced treatment to patients. The challenge for these systems is in focusing the ideal dosage and intensity of radiation on the tumour itself while minimizing radiation exposure to surrounding tissues and organs.

MacDonald, with one of the existing Brainlab accelerators in Halifax. (File photo)
What MacDonald has been researching, together with Drs. Thomas and Robar, is an algorithm that condenses the wealth of information about the patient and their disease and formats it in such a way that BrainlabŌĆÖs software is able to move the patientŌĆÖs bed dynamically during radiation treatment. These software plans, customized for each patient, amount to whatŌĆÖs known as a ŌĆ£Four-PiŌĆØ approach to trajectory-based treatment planning. The result: the radiation is focused, to the greatest degree possible, on the tumour itself.
ŌĆ£By moving healthy structures away from the path of incident radiation, we are further reducing the probability of healthy tissue damage as part of treatment,ŌĆØ explains MacDonald. ŌĆ£It represents a step forward in patient-specific treatments and patient safety.ŌĆØ
The power of partnership
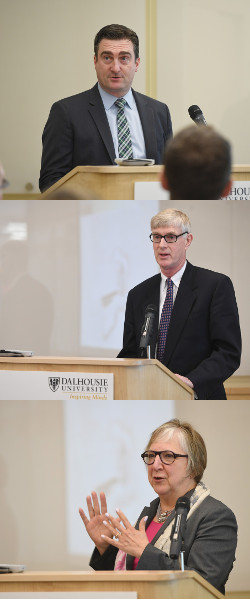
At Wednesday morningŌĆÖs announcement event in the Life Sciences Research Institute, the various partners involved in the project gathered to celebrate the licensing agreement and the commercializing of the research. ┬Ā
ŌĆ£WeŌĆÖre excited to incorporate ┬ķČ╣┤½├ĮŌĆÖs Four-Pi approach, and its unique trajectory-based planning program for delivery, as part of our next generation of Brainlab cranial radiosurgery software thatŌĆÖs scheduled for release within the year,ŌĆØ said Brainlab President Sean Clark.
ŌĆ£The world of cancer care is really changing under our feet,ŌĆØ said Dr. Drew Bethune, medical lead for the Provincial Program of Care for Cancer for the Nova Scotia Health Authority. ŌĆ£Some equate these machines to ŌĆśsmart bombsŌĆÖ or laser-guided missiles, and thatŌĆÖs really understating it: these are much more precise than thatŌĆ” I canŌĆÖt wait for this technology to be available. This will affect every patient in the world.ŌĆØ
Marta Crago, vice-president research at ┬ķČ╣┤½├Į, celebrated the technology as a great example of how local innovation, through partnership, can lead to a commercial product that makes a difference in peopleŌĆÖs lives.
ŌĆ£Research partnerships like this are important,ŌĆØ she said. ŌĆ£TheyŌĆÖre important for translating basic science into medical science into patient care ŌĆöinto something that offers outcomes for graduate students, outcomes for people around the world facing health issues, and economic outcomes as well.ŌĆØ
Commercialization success
Singled out for particular thanks during remarks was the team at , who worked with the inventor team to file intellectual property protection and with Brainlab to finalize the license agreement. ŌĆ£ItŌĆÖs really an incredible resource to have here,ŌĆØ said Dr. Robar of the office and its staff.
For MacDonald, the experience of working with his faculty collaborators, the ILI office and Brainlab to commercialize this research has made for an experience heŌĆÖll carry with him through his entire career.
ŌĆ£As a gradate student, I certainly recognize how fortunate I am to be part of this [research] group, and the experience of building this work and engaging industry partners has introduced me incredible opportunities I could have never hoped to be a part of.ŌĆØ

All images: Danny Abriel